 One thing we learned during the COVID 19 pandemic was the value of telehealth. Patients could see their physician from home, avoiding the danger of infection – and also eliminating the transportation barrier that many of our patients struggle with. We also quickly came face to face with its limitations. For example, we couldn’t measure blood pressure, which made management of patients’ hypertension difficult.
One thing we learned during the COVID 19 pandemic was the value of telehealth. Patients could see their physician from home, avoiding the danger of infection – and also eliminating the transportation barrier that many of our patients struggle with. We also quickly came face to face with its limitations. For example, we couldn’t measure blood pressure, which made management of patients’ hypertension difficult.
The exciting news is that recent innovations have made it possible for patients to track their own blood pressure with wi-fi enabled blood pressure cuffs.
In May 2021, ChesPenn launched our self-monitoring blood pressure management program with funding from a grant provided by the Health Resources and Services Administration (HRSA) and assistance from the Health Federation of Philadelphia. Patients receive instructions in taking their blood pressure and are asked to record measurements twice in the morning and twice in the evening. Patient Engagement Specialist Amyah Blakely reviews results daily that feed into a portal and then reports them to each patient’s provider through the EMR.
In May 2021, ChesPenn launched our self-monitoring blood pressure management program with funding from a grant provided by the Health Resources and Services Administration (HRSA) and assistance from the Health Federation of Philadelphia. Patients receive instructions in taking their blood pressure and are asked to record measurements twice in the morning and twice in the evening. Patient Engagement Specialist Amyah Blakely reviews results daily and reports them to each patient’s provider. When providers see elevated results, they can adjust the patient’s medication until the blood pressure returns to a healthy level. This means patients don’t have to wait months for their next visit to have their provider check their blood pressure and make any changes needed. To date, we have distributed blood pressure cuffs to over 250 patients and our goal is to expand the program to every patient whose blood pressure is not well controlled.
Patients have embraced their new ability to monitor their blood pressure. The cuffs include an app that patients can download to their phones so that they can also keep track of both blood pressure and heart rate. We’ve found that this tool helps increase patients’ engagement in their health management.
This initiative provides a powerful new tool for our participation in the Million Hearts® Collaboration. Million Hearts® is a national collaboration co-led by the Center for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS).
Current priorities for the program include optimizing care with blood pressure control. 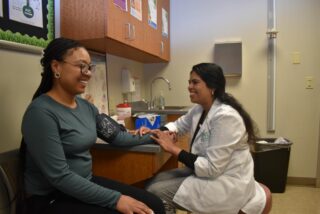
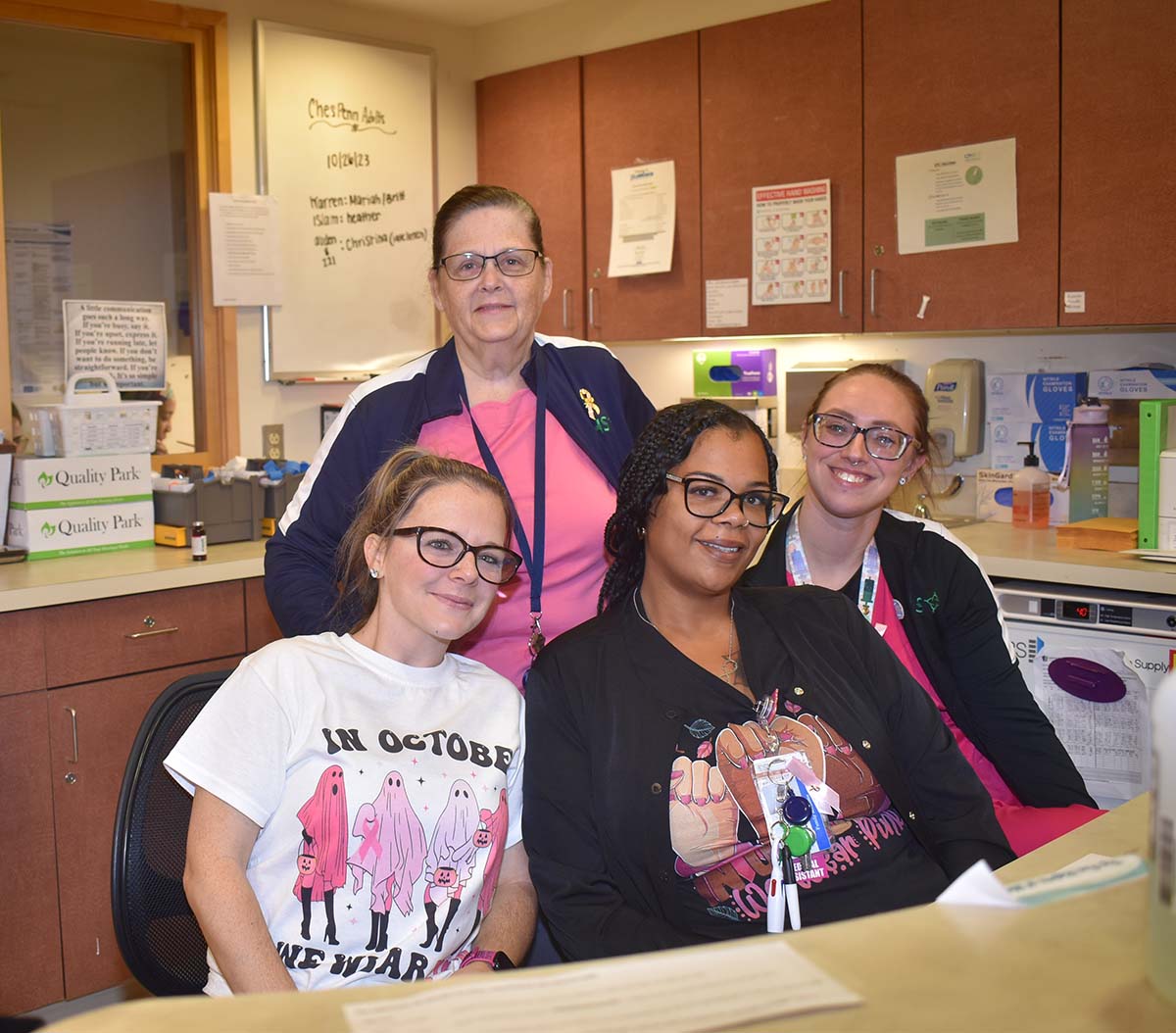
ChesPenn Chief Medical Officer Dr. Letitia O’Kicki commented on the program that, “The Million Hearts® project has been a very important program advancing health equity and contributing to the health of the communities we serve. Through team-based care and evidence-based guidelines, blood pressure is closely monitored and medication added or adjusted, if needed. The focus has been to better control blood pressure in our patients, preventing strokes and heart attacks. Self-monitoring blood pressure machines have allowed patients to be very engaged in their health care. Our team-based approach includes the clinical care team: providers, nurses, medical assistants, health educator, behavioral health consultant, pharmacist, and the quality improvement team, along with the patient engagement specialist.”
During our 50th anniversary year, we’ve focused on celebrating 50 years of caring for the communities we serve while looking to the future, exploring innovative strategies to meet our patients’ evolving needs. This new program is a wonderful glimpse into the possibilities for community health care in the coming years.






 As a little girl, DaNesha Mack was fascinated by germs and knew she wanted to work in healthcare. She thought she might want to be a doctor. In college she was able to explore different aspects of health and medicine and found her niche in public health. She started to study health equity and took courses in health and social justice.
As a little girl, DaNesha Mack was fascinated by germs and knew she wanted to work in healthcare. She thought she might want to be a doctor. In college she was able to explore different aspects of health and medicine and found her niche in public health. She started to study health equity and took courses in health and social justice. Penn Medicine Chester County Hospital is offering a COVID-19 update at the Equity Health Center and online on Monday, December 11, 2023 from 12:00 – 1:00 PM.
Penn Medicine Chester County Hospital is offering a COVID-19 update at the Equity Health Center and online on Monday, December 11, 2023 from 12:00 – 1:00 PM.







 One thing we learned during the COVID 19 pandemic was the value of telehealth. Patients could see their physician from home, avoiding the danger of infection – and also eliminating the transportation barrier that many of our patients struggle with. We also quickly came face to face with its limitations. For example, we couldn’t measure blood pressure, which made management of patients’ hypertension difficult.
One thing we learned during the COVID 19 pandemic was the value of telehealth. Patients could see their physician from home, avoiding the danger of infection – and also eliminating the transportation barrier that many of our patients struggle with. We also quickly came face to face with its limitations. For example, we couldn’t measure blood pressure, which made management of patients’ hypertension difficult.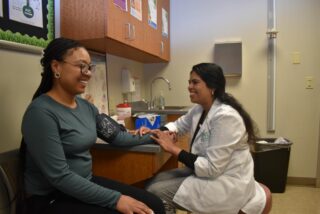







 Letitia O’Kicki grew up in a small town in western Pennsylvania. The eldest of 7 siblings, caring for others came naturally and her maternal uncle, who was a family medicine physician, also had a profound impact on her. “We had this close relationship so when I went to Penn as an undergrad and Temple medical school and began to take rotations I would go back home and take them with my uncle in his office. He was very warm, very tender, very nurturing and had a really wonderful relationship with his patients. He took care of generations of families which was really nice to see. When a woman went into labor in a in a snowstorm someone would come on a snowmobile to take him to deliver the baby. He was just a great role model and mentor.”
Letitia O’Kicki grew up in a small town in western Pennsylvania. The eldest of 7 siblings, caring for others came naturally and her maternal uncle, who was a family medicine physician, also had a profound impact on her. “We had this close relationship so when I went to Penn as an undergrad and Temple medical school and began to take rotations I would go back home and take them with my uncle in his office. He was very warm, very tender, very nurturing and had a really wonderful relationship with his patients. He took care of generations of families which was really nice to see. When a woman went into labor in a in a snowstorm someone would come on a snowmobile to take him to deliver the baby. He was just a great role model and mentor.” “I really love what I do. Doctor Yagnik laid a strong foundation, and we want to build it higher and stronger and with Sue (Susan Harris McGovern) as CEO we have a really nice team.” Under Dr. O’Kicki’s direction, ChesPenn participates in nationally recognized programs including the American Heart Association’s Million Hearts Program and Crucial Catch, a collaboration with the American Cancer Society and the NFL. The leadership team is also exploring possible new collaborations with major health care systems in the region, made possible in part because of Dr. O’Kicki’s academic appointments at Drexel and Temple Universities.
“I really love what I do. Doctor Yagnik laid a strong foundation, and we want to build it higher and stronger and with Sue (Susan Harris McGovern) as CEO we have a really nice team.” Under Dr. O’Kicki’s direction, ChesPenn participates in nationally recognized programs including the American Heart Association’s Million Hearts Program and Crucial Catch, a collaboration with the American Cancer Society and the NFL. The leadership team is also exploring possible new collaborations with major health care systems in the region, made possible in part because of Dr. O’Kicki’s academic appointments at Drexel and Temple Universities.



